On January 14, 2020, Guangyu Zhou’s team from School of Psychological and Cognitive Science of Peking University published a paper “HIV Disclosure to Family Members and Medication Adherence: Role of Social Support and Self‑efficacy” in the journal of AIDS and Behavior. The study revealed the mediating role of social support and self-efficacy underlying the relationship between HIV disclosure to family members and antiretroviral therapy (ART) adherence.
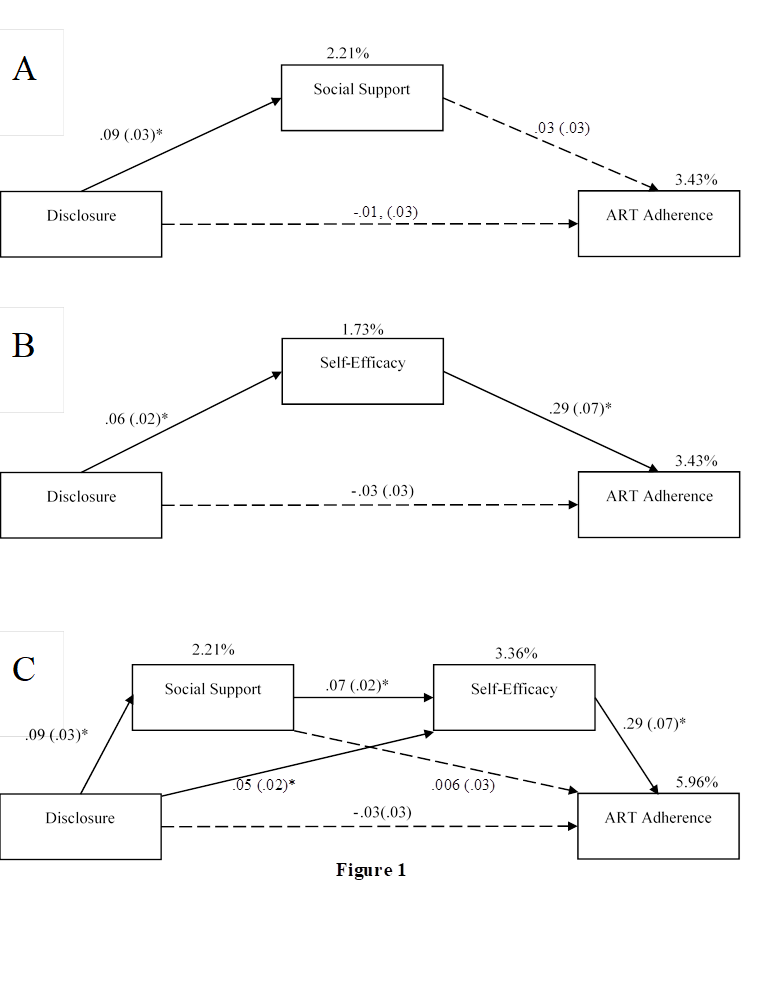
ART is vital to people living with HIV (PLWH) by suppressing the virus and in turn preventing onward HIV transmission and reducing AIDS-related morbidity and mortality. Optimal adherence is often considered as 95% or more of prescribed doses taken, but the adherence rates continue to remain low with only 61%–83% across various cultural settings. ART adherence is influenced by many factors, including personal attributes, institutional resources, treatment related factors, and psychosocial factors. Among these factors, disclosure of HIV status is considered to be a critical predictor of ART adherence. However, few studies have explored the mechanisms underlying the association between HIV disclosure and medication adherence. The Disclosure Process Model posits that multiple processes exist between disclosure and clinical outcomes, and social support is one of the potential mediators explaining the effect of disclosure on adherence. Besides, the significant association between medication self-efficacy and ART adherence has been reported in a number of studies. According to the Social Cognitive Theory, individuals who have higher self-efficacy to perform health promoting behavior are more likely to do so. Thus, it is plausible to hypothesize that treatment self-efficacy might play a mediation role between disclosure and adherence. The Social Cognitive Theory indicates that social support is likely to engender self-efficacy beliefs, which in turn improve health outcomes, so the serial (“chain”) mediating effect was also tested in the current study.
Data of the current study was collected from PLWH in China, and the path analyses revealed that disclosure to family members had significant indirect effects on adherence via social support and self-efficacy (figure 1). Our findings suggested that HIV disclosure might positively affect ART adherence through two psychosocial pathways: social support and self-efficacy. Future intervention to improve medication adherence among PLWH should consider targeting these two factors.
Tianyue Mi from School of Psychological and Cognitive Sciences, Peking University, was the first author of the article. Guangyu Zhou, the assistant professor (in tenure-track) at Peking University, was the corresponding author. Professor Xiaoming Li and Shan Qiao from University of South Carolina Arnold School of Public Health contributed to this paper. The work was funded by National Institutes of Health and National Nature Science Foundation of China.


